Short(ish) and sweet summary of what I learned in MHST 601.. I could ramble all day..
- Jessica Byrne
- Apr 8, 2021
- 8 min read

Introduction
Foundations of Health Systems in Canada course has really helped me to understand health care in Canada and the differences between provinces/territories, vulnerable populations, and rural/urban areas. Until this course I hadn't realized how intricate the Canadian health care system is and the gaps that exist even in our “universal” system.
At first I wasn’t certain what to focus on but as the course continued and I learned more from social media, classmates, and resources, I settled on one of our most vulnerable populations: seniors and their care in Canada, and the drastic improvements that need to be made.
Professionalism
Before we evaluated the system, we looked at ourselves and how we work within our scope. As a registered nurse I have professional standards to abide by via the College of Registered Nurses of Newfoundland and Labrador and the Canadian Nurses Association. I have started to understand what is considered professional and appropriate for a digital presence in both personal and professional lenses, and how to portray my professional credentials, coursework, and curated resources through an e-portfolio.
What’s health?
One of the things that I have learned from my classmates and resources is that the World Health Organization's (WHO) definition of health: “a state of complete physical, mental and social well-being and not merely the absence of disease.“ (WHO, 1948), is not completely wrong, but it is not in line with our current population and health care demands.
There is a lot of focus on the aspects of health but not what causes people to be "unhealthy". A more modern definition of health is: “Our vision of health is that any individual in society is able to live the best life possible according to what they value, facilitated by access to high quality, patient-centered, evidence based and affordable health and care services and supported by a strong public health system.” (Gentry, S, Badrinath, P., 2017).
Many definitions of health stem from the Canada Health Act (CHA), which is out of touch with current health care needs. When the CHA was developed in 1984 the focus was on acute and physician focused, medically necessary/essential care. CHA should be updated to include universal pharmaceutical coverage, long-term and home care, dental care, and mental health and addictions services. There also needs to be an evaluation on what is considered "medically necessary" as our population ages and chronic illness bares a major burden on our system.
Social Determinants
Some work done in NL around the SDH with the "Healthy People, Healthy Families, Healthy Communities Framework", (Department of Health and Community Services, 2014), as well as the "Health Accord for NL: 10-year Health Transformation" (Health Accord, 2020). We certainly need to work towards what we discussed in the last unit about re-defining what health is, and modernize the health care act to promote equity and accessibility. I have learned so much from my classmates' knowledge and experiences about the social determinants of health and how people’s lives and health are affected by way more than just physical and mental aspects. “The primary factors that shape the health of Canadians are not medical treatments of lifestyle choices but rather the living conditions they experience.” (Mikkonen, J., Raphael, D., 2010).

Much of the information about the social determinants discusses the astronomical amount of money being spent on health care and the lack of money being spent on social issues. For example: in NL since 1981 we have increased health care spending by 232% while social spending has only increased by 6% (Health Accord, 2020). This was not uncommon from what I discussed and read with classmates from other provinces. The WHO’s Commission on Social Determinants of Health (CSDH) states:
“Certainly, maldistribution of health care – not delivering care to those who most need it – is one of the social determinants of health. But the high burden of illness responsible for appalling premature loss of life arises in large part because of the conditions in which people are born, grow, live, work, and age. In their turn, poor and unequal living conditions are the consequence of poor social policies and programmes, unfair economic arrangements, and bad politics. Action on the social determinants of health must involve the whole of government, civil society and local communities, business, global fora, and international agencies.” (Commission on Social Determinants of Health, 2008).
Model of Health

I focused on the Population Health Promotion Model in relation to chronic illness and health status and it says we need to look at the who, the what and the how. We need to look at who utilizes the health care system, why they use it, and how. An example: a senior who lives alone and has diabetes, congestive heart failure and arthritis, utilizes the ER “inappropriately” to seek medication refills and health advice because he has no primary care provider. The population health model would say to expand and promote primary health care to ensure that people have access to the most appropriate care provider when they need it.
The Department of Health and Community Services (2015) stated “In Newfoundland and Labrador, primary health care is typically a person’s first point of contact with the health care system. It encompasses a range of community-based services essential to maintaining and improving health and well-being throughout an individual’s entire lifespan. It includes services that promote health and wellness, prevent illness, treat health issues or injuries, and diagnose and manage chronic health conditions”.
Chronic Illness
MHST 601 then led us to look at chronic diseases, and although diabetes, heart disease, chronic obstructive pulmonary disease (COPD), cancer, and other chronic diseases continue to be of high priority for care providers and government, they cannot be truly addressed without looking at individual’s whole health.

The Chronic Disease Action Plan set out by government frameworks initiatives of prevention, self-management, and treatment and care. These can guide care providers to engage in high quality, person-focused care, and provide individuals with the education and assets needed to achieve their personal health goals (Chronic Disease Action Plan, 2017).
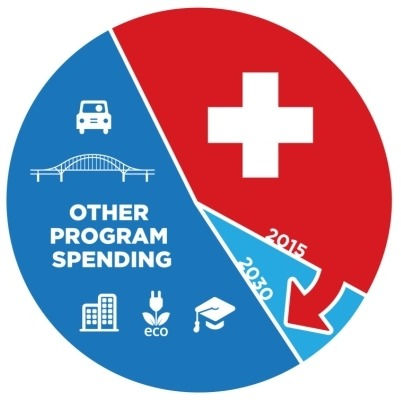
According to WHO, 7/10 people (41 million) worldwide die from cardiovascular diseases, cancer, diabetes and chronic lung diseases annually. More than 85% of these “premature” deaths occur in low and middle-income countries. Over the next 15 years the costs of chronic diseases are predicted to reach more than $7 trillion USD in developing countries alone.
I realize now after reading many articles, documents, and sharing discussions with my course mates that there are many factors that drive the social determinants of health that affect those living with or who are at risk for chronic diseases.
Indigenous/Vulnerable Populations

To look at vulnerable populations we were first asked to focus on indigenous peoples.
As a registered nurse I am bound by professionalism to promote equal, fair and judgement-free care. My governing body, the College of Registered Nurses of Newfoundland and Labrador states: “We call upon those who can effect change within the Canadian health-care system to recognize the value of Aboriginal healing practices and use them in the treatment of Aboriginal patients in collaboration with Aboriginal healers and Elders where requested by Aboriginal patients” (CRNNL, 2019).
Some of the things I learned from this unit include: Jordan’s principle, the horrifying information around the missing and murdered indigenous women and girls, the repercussions of the Indian Act, the mental and physical trauma the residential schools have had on generations of indigenous peoples, and the health disparities including access, racism, barriers, mental health and addictions, the social determinants of health, and how they affect the health and chronic disease rates of the aboriginal populations.
Some other vulnerable populations include children, single parents, the homeless, sex workers, and visible minorities just to name a few, but for the purpose of this unit and this course I chose to focus on seniors. I was shocked to discover the staggering rates of the aging population. WHO stated that the number of people worldwide who are 65+ is estimated to grow from around 524 million in 2010 to almost 1.5 billion in 2050 (WHO, 2011). In Canada it is predicted that up to 25% of the population will be over 65 in 2036.
Covid-19 showed the public what many of us have known for years: the LTC and home care sectors need a complete overhaul. Some of the common concerns are:
· Lack of acknowledgement from government that the aging population is growing quickly and we need to address it now.
· The serious gap between funding and support for home care vs LTC (for every $1 spent on home care there are $6 spent on LTC).
· Unsafe staffing levels.
· Outdated care models (ie: the Canada Health Act).
· Failure to support families and care givers to enable individuals to stay in their own homes.

Some of the recommendations the Canadian Nurses Association made for the Aging and Seniors Care Commission of Canada (ASCCC) to address the care of our rapidly aging population include:

· Promotion of health and well-being of all Canadians as they age
·Chronic disease prevention and management resources.
· Increase system capacity around frailty and vulnerability.
Future Directions
Focusing on a future direction for the final unit was difficult, as there are so many important ones. I decided to stick with something I am passionate about and look at what we need to do to improve the care of seniors. We need to drastically change how we care for seniors and the money that is being spent on a system that is broken. By promoting home and community care, we can actually save money.

Some of the other future health focuses include e-health and virtual care, pandemic planning, and both infectious and non-communicable disease prevention and education. I think we are definitely headed into a more virtual world and from my experience that could be a good thing. For vast, rural areas like NL, virtual care could be greatly utilized to help people get easier access to care providers and for care providers and utilize electronic health records and telemedicine to appropriately care for patients.
Conclusion
This course has provided me with opportunities to learn about the social determinants of health, provincial/territorial and federal levels of health services and how they are all so closely interconnected. I have learned so much about different areas, groups, and services that I did not know about and I now have a greater understanding of our health care system, what works really well and how it could be improved. Something that stands out to me is the need for the modernization of the Canada Health Act, improvements to LTC and home care funding and standards, support for those vulnerable populations such as indigenous peoples and seniors, and how health care professionals can be the voice and fighters for what the people of Canada deserve.
References
Canadian Nurses Association. (2013). Three Strategies to help Canada's Most Vulnerable (Canada). Ottawa, ON.
College of Registered Nurses of Newfoundland and Labrador. (2021, January 14). Standards of Practice for Registered Nurses and Nurse Practitioners. CRNNL. https://
CSDH (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva, World Health Organization.
Department of Health and Community Services, Healthy people, healthy families, healthy communities: A primary health care framework for Newfoundland and Labrador 2015-2025 (2015). St. John's, NL.
Department of Health and Community Services, Department of Health and Community Services Strategic Plan 2017-2020 (2017). St. John's, NL.
Department of Health and Community Services, The Way Forward: Chronic Disease Action Plan (2018). St. John's, NL.
Gama e Colombo, D. (2010). Closing the gap in a generation: Health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Revista de Direito Sanitário, 10(3), 253. https://doi.org/10.11606/issn.2316-9044.v10i3p253-266
Gentry, S., & Badrinath, P. (2017). Defining Health in the Era of Value-based Care: Lessons from England of Relevance to Other Health Systems. Cureus. https://doi.org/10.7759/cureus.1079
Health Accord for Newfoundland and Labrador. (2021). (rep.). A 10-year health transformation. Retrieved from https://healthaccordnl.ca/
Health Canada. (2020, February 24). Canada Health Act. Retrieved April 1, 2021, from https://www.canada.ca/en/health-canada/services/health-care-system/canada-health-care-system-medicare/canada-health-act.html
Lee, K., Koivusalo, M., Ollila, E., Labonté, R., Schrecker, T., Schuftan, C., & Woodward, D. (2007). WHO Commission on Social Determinants of Health Globalization, Global Governance and the Social Determinants of Health: A review of the linkages and agenda for action. https://www.who.int/social_determinants/resources/gkn_lee_al.pdf.
Mikkonen, J., Raphael, D., York University (Toronto, Ont. ), & School of Health Policy and Management. (2010). Social determinants of health: The Canadian facts. York University School of Health Policy and Management. http://books.scholarsportal.info/viewdoc.html?id=/ebooks/ebooks0/gibson_cppc/2010-08-06/6/10390848
Public Health Agency of Canada. (2011, October). World Conference on Social Determinants of Health. Rio de Janeiro.
World Health Organization, Health and Welfare Canada, & Canadian Public Health Association, Ottawa Charter for Health Promotion (1986). Ottawa, ON.




Comments